You notice your heart races without warning, even when you’re resting quietly at home
It’s not panic. Not excitement. Just an irregular beat. Sudden. Unpredictable. Your chest flutters like wings beneath your ribs. Sometimes it slows. Sometimes it quickens. But it’s never calm. You sit still, but your pulse acts like it’s running. That’s often how atrial fibrillation starts—no grand entrance, just quiet chaos inside your chest.
You feel tired in a way sleep doesn’t fix—and the fatigue seems to come from nowhere
You slept eight hours. Ate well. Yet you feel drained. Your energy evaporates by mid-morning. Small tasks feel big. Your limbs feel heavier than usual. Atrial fibrillation disrupts how efficiently your heart moves blood. That inefficiency shows up as fatigue, not pain. It’s like running a marathon on low fuel—even if your legs never move.
There’s a flutter in your chest that comes and goes—but you can’t predict when or why
One minute you’re fine. The next, you feel your heart jump. Then nothing. Then again. It’s not painful, but it’s unnerving. You wait for it to pass. You search for patterns. Caffeine? Stress? Sleep? Sometimes there is a trigger. Often, there isn’t. That unpredictability is part of what makes atrial fibrillation so dangerous—and easy to ignore.
Your doctor hears something irregular and sends you for an ECG—even though you feel mostly fine
You went in for something routine. A checkup. A cough. They listen and pause. The stethoscope lingers. Then comes the suggestion—let’s run an ECG. That’s where it shows. Irregular rhythm. Rapid beats. The test catches what the body sometimes hides. You thought you were just tired. But your heart was already signaling distress.
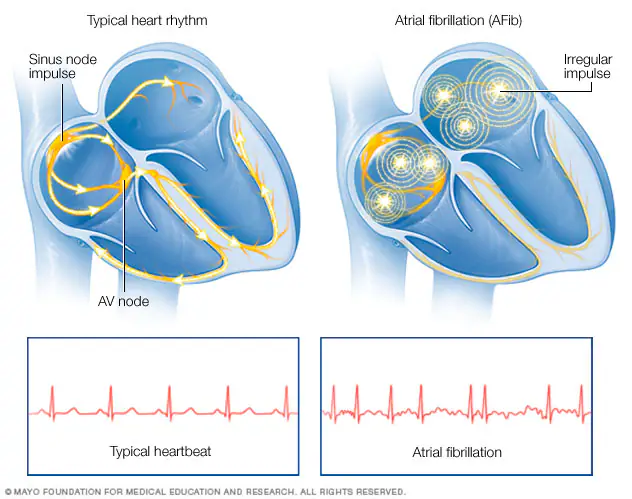
You’ve been told your atria are misfiring—sending signals out of sync, causing the flutter
Atrial fibrillation isn’t about blockage. It’s about rhythm. Your atria—the upper chambers—don’t contract properly. They quiver. Signals misfire. Blood flow becomes turbulent. Clots can form. Strokes can follow. It’s not just a heartbeat issue—it’s a circulation issue. That’s why treatment is about more than comfort—it’s about protection.
Your symptoms worsen when you’re dehydrated, anxious, or after alcohol—and you’re beginning to notice a pattern
You track your habits. You see the connection. One glass of wine, and the flutter returns. A stressful day, and your heart speeds. These aren’t coincidences. Certain triggers worsen atrial fibrillation episodes. Learning those patterns becomes part of the treatment. Awareness doesn’t solve it—but it softens the surprise.
Your options include medication, but each comes with its own risks, adjustments, and monitoring
Beta-blockers. Calcium channel blockers. Blood thinners. Each comes with instructions. Dosage. Timing. Side effects. You start one, then adjust. Then another. You’re not just treating the rhythm. You’re managing risk. Preventing stroke. Slowing the heartbeat. Each step must be measured, because balance matters more than speed.
You’re offered a procedure called cardioversion—an attempt to restore normal rhythm with electrical pulses
The idea feels strange—electricity to the heart. But it’s targeted. Short. Controlled. They sedate you. The shock is brief. The hope is reset. It works for many. But not all. Some rhythms return. Some hearts resist. Still, it’s a step—one of many in the journey toward calm.
Catheter ablation is mentioned when medication fails—and you learn about targeting faulty tissue directly
Ablation means precision. A catheter enters through a vein. Finds the problem spots. Destroys them. Carefully. With heat or cold. It’s invasive but focused. Aimed at stopping the triggers at their source. Recovery isn’t instant. But for many, it brings real relief. Not a cure, but a reprieve.
You start hearing about stroke risk—and how even silent episodes can lead to serious consequences
You didn’t think it was that serious. Just flutters. But now you hear the word stroke. Blood pooling in the atria can clot. Those clots travel. Atrial fibrillation increases stroke risk fivefold. That’s why treatment includes blood thinners, even when symptoms feel mild. Because consequences don’t wait for pain to be loud.
